
Immersive technologies such as virtual reality (VR) and augmented reality (AR) have seen a recent explosive evolution of applications for medical education. It is now becoming practical to incorporate this technology to teach nursing, medical, and other health professions students. This continues a long tradition of experiential training. While incorporating new technology is exciting, it is important to understand the educational theory behind its implementation to create the best curriculum for students. Core educational theories that have shaped current simulation-based curriculums include behaviorism, constructivism, social-constructivism, and experiential learning (McGaghie 2018).
One of the earliest education theories, behaviorism describes how students’ respond and adapt to their environment. For a pure behaviorist, the focus is on what students do, and not how they think or feel (Kay, 2016). This theory is teacher centered. Teachers control the environment, identifying appropriate rewards and/or punishments to reinforce desired behaviors. While modern educational theory has certainly moved beyond pure behaviorism, it has had lasting contributions on educational framework including direct teaching, role of incentives and rewards, the importance of clarifying learning objectives, and behavior management (Kay, 2016).
Constructivist learning theory sees knowledge as subjective and actively constructed as learners engage with, and make meaning of, their lived experience (Kay, 2016). Instead of knowledge being an objective fact that the teacher holds and shares with the learner, constructivists believe knowledge is subjective. The learner builds their knowledge through subjective experiences and in the context of previous life experiences. This paradigm shift to contructivist learning theory was in large part due to Jean Piaget’s research on children’s cognitive development. Teaching strategies include more student-centered instruction designed to engage students in constructing their own personal knowledge. Lessons are designed to take place in real-world situations where students are presented with complex problems. Social constructivism takes this idea further to say that students live in a social context that guides their perspective, learning in the context of their lived experiences in society.
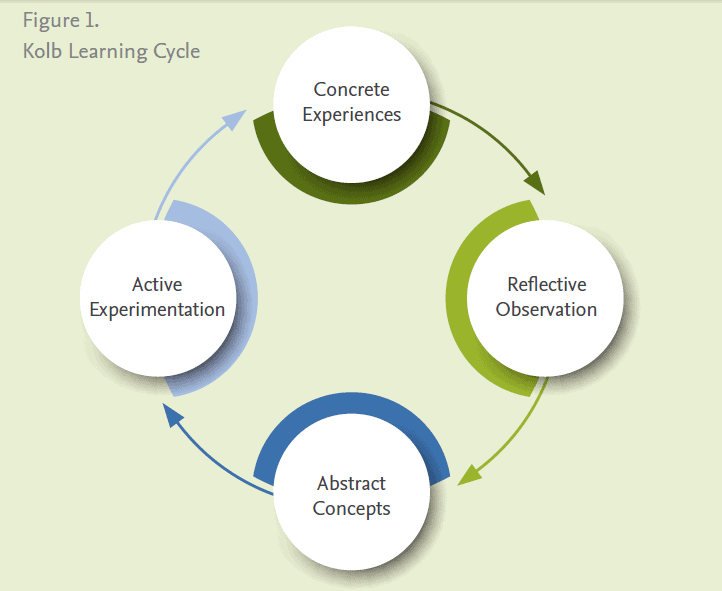
Another learning theory put forth by Kolb and Fry is the experiential learning cycle. Building on previous theories, they explained that learning happens in a continuous loop from concrete experiences, to reflective observation of experiences, to formation of abstract concepts, to testing new concepts, which make more concrete experiences. Students can enter the cycle at any point, and this process can happen quickly or over time (Kolb, 1984).
The foundational learning theories have influenced modern healthcare education. Most programs have moved to providing students with early clinical exposure, with the intent that this real-life experience will provide a student-centered, rich learning environment. However, putting learners in a real clinical environment can lead to errors affecting patient care. These less controlled environments may also leave opportunity for inappropriate student stress and trauma that could have negative learning consequences.
To balance these challenges of experiential learning in a clinical setting, simulation-based learning gives students exposure to real-life experiences without the risks of patient harm. Simulation learning has been shown to enhance transfer of learning, specifically allowing students to take on the roles of what will be expected of them in practice (Miles, 2018). Until recently, manikin-based simulation was the most common available option for high fidelity, realistic simulation. But now with the technological advances in VR and AR, immersive technologies can augment or replace manikin-based simulation to provide an engaging and interactive real-life experience (Izard, 2018; Kyaw, 2019; Ellington, 2019; Sapkaroski, 2019).
Read more: Helpful Resources for Understanding Virtual Reality Simulations and Application in Nursing EducationImmersive technology provides many advantages over more traditional types of simulation. The most pressing advantage in our times is the ability to host remote learning activities. Many immersive platforms allow the educator and students to be in real-life separate spaces, while still participating in the same virtual simulation. Scenarios can also broadcast in real-time to a larger student audience who can participate through observation. Remote learning also gives the opportunity to invite expert guest educators. For instance, a nationally renowned cardiology educator could serve as a remote moderator for an ACLS simulation. Immersive technologies also allow for more control over the development of scenarios. For instance, the educator can decide the amount of visual realism needed to teach a specific topic. They can design the cases to be fully immersive or partially immersive to allow for hints or other guidance through a case. There is also the ability to program cases to run with a moderator to guide case flow, or instead allow the student to play through the scenario like a video game without a moderator. This can allow for a wide range of case complexity. Educators could design either basic scenarios students complete asynchronously, or instead develop highly complex scenarios with dynamic case flow and multiple potential outcomes.
For educators considering implementing immersive technologies, first consider a few basic principles. Most importantly, set out clear learning objectives. Once established, determine if virtual reality is the right technology to help teach these learning objectives. The best applications of this technology leverage the unique strengths of VR such as the ability to provide remote learning or increased visual realism. Also consider the practical application of the technology during the learning activity, such as if students will complete the scenarios individually or in groups and how to include extra students that cannot actively participate in the scenario. Careful planning that is grounded in clear learning objectives before implementation will allow the technology implementation to be successful.
References
Ellington, D. R., Shum, P. C., Dennis, E. A., Willis, H. L., Szychowski, J. M., & Richter, H. E. (2019). Female Pelvic Floor Immersive Simulation: A Randomized Trial to Test the Effectiveness of a Virtual Reality Anatomic Model on Resident Knowledge of Female Pelvic Anatomy. Journal of Minimally Invasive Gynecology, 26(5), 897–901. https://doi.org/10.1016/j.jmig.2018.09.003
Izard, S. G., et al. (2018). “Virtual Reality as an Educational and Training Tool for Medicine.” J Med Syst 42(3): 50
Kay D, Kibble J. Learning theories 101: application to everyday teaching and scholarship. Adv Physiol Educ. 2016 Mar;40(1):17-25. doi: 10.1152/advan.00132.2015
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development (Vol. 1). Englewood Cliffs, NJ: Prentice-Hall
Kyaw, B. M., Saxena, N., Posadzki, P., Vseteckova, J., Nikolaou, C. K., George, P. P., … Tudor Car, L. (2019). Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. Journal of Medical Internet Research, 21(1), e12959. https://doi.org/10.2196/12959
McGaghie WC, Harris IB. Learning Theory Foundations of Simulation-Based Mastery Learning. Simul Healthc. 2018 Jun;13(3S Suppl 1):S15-S20. doi: 10.1097/SIH.0000000000000279. PMID: 29373384
Miles DA. Simulation Learning and Transfer in Undergraduate Nursing Education: A Grounded Theory Study. J Nurs Educ. 2018 Jun 1;57(6):347-353. doi: 10.3928/01484834-20180522-05. PMID: 29863735.
Sapkaroski, D., Baird, M., Mundy, M., & Dimmock, M. R. (2019). Quantification of Student Radiographic Patient Positioning Using an Immersive Virtual Reality Simulation. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 14(4), 258–263. https://doi.org/10.1097/SIH.0000000000000380